At Week 4, a look at key EM legislation in Virginia
Today wraps the fourth of nine weeks at the 2026 Virginia General Assembly, and VACEP’s government affairs team and leadership are actively tracking dozens of bills that touch either emergency medicine or the general house of medicine. Here’s a look at a few of the key bills and where they stand.
Bills VACEP Supports
Keep patients who lack consent safely in the ER when they have a critical medical need | HB309 (Hope)
Under current Virginia law, physicians must obtain a court- or magistrate-issued medical Temporary Detention Order (TDO) to treat patients who cannot consent to care due to conditions such as intoxication, delirium, or hypoxia. However, the law does not clearly define who has custody of a patient during the critical window between arrival in the ER and issuance of that order.
Introduced by VACEP, the bill clarifies that while a medical TDO is being sought, a patient who lacks capacity is to remain in the custody of the hospital, allowing security staff to prevent the patient from leaving for a limited period. The bill does not expand detention authority, extend the duration of a TDO, or create new standards for involuntary treatment, and preserves existing liability protections for clinicians acting in good faith.
Status: Passed the Health and Human Services committee with unanimous support.
Emergency physicians with Mark Downey, M.D. at EM Advocacy Day. Downey, whose district covers York County and surrounding areas, is the only doctor in the General Assembly after winning election in November.
Improving the review and disciplinary process for Board of Medicine complaints | HB1139 (Downey)
Introduced by VACEP, the bill modernizes the makeup of Virginia’s Board of Medicine. Currently, the board is the only health regulatory board in the Commonwealth required by statute to appoint physician members based on congressional districts rather than clinical expertise.
That structure can limit specialty representation on a board that primarily handles disciplinary complaints and standard-of-care reviews.
The proposed change would remove the geographic requirement and allow appointments based on medical licensure, improving access to specialty expertise without altering the board’s authority or mission.
Status: Passed the Health and Human Services committee (21‑Y 1‑N)
Banning non-competes for healthcare workers | HB627 (Helmer) & SB128 (VanValkenburg)
Emergency physicians are supporting legislation to ban non-compete agreements for healthcare providers. The argument: non-compete clauses worsen Virginia’s existing physician shortage by forcing clinicians to leave communities entirely when employment relationships end, disrupting access to care and continuity for patients.
Virginia already faces a shortage of nearly 4,000 doctors. Limiting where clinicians can practice only exacerbates delays in specialty coverage and transfers — problems felt acutely in emergency departments.
Status: Both bills are moving forward through the House and Senate with near complete support.
Virginia emergency physicians on the steps of the General Assembly Building at EM Advocacy Day on January 28 in Richmond. There, they expressed support and voiced opposition for various pieces of legislation under consideration.
BILLS VACEP OPPOSES
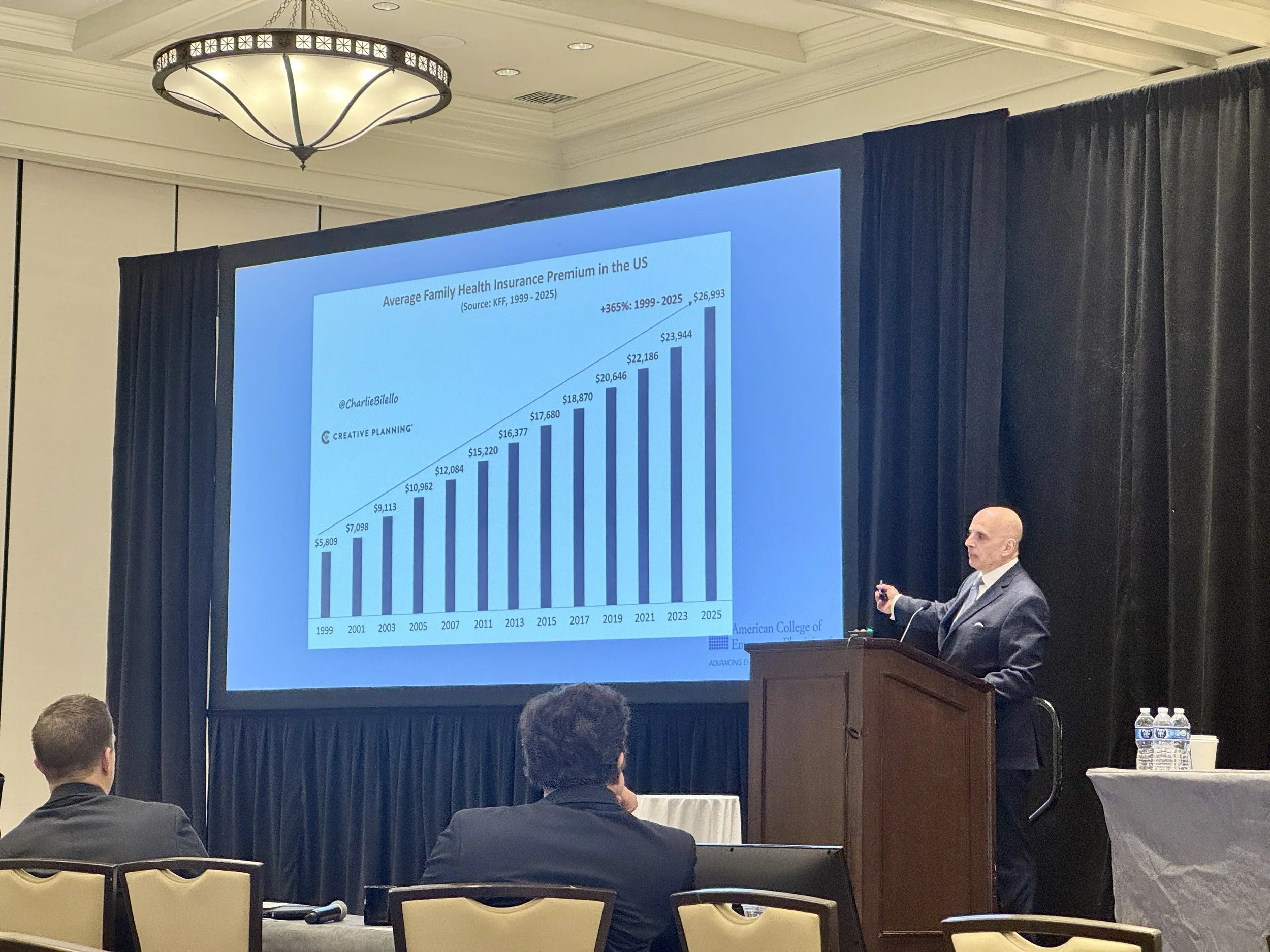
Increasing the medical malpractice cap | SB99 (Stanley)
The bill would eliminate Virginia’s medical malpractice cap for patients age 10 and younger. Virginia’s medical malpractice cap is $2.7 million, and increases by $50,000 each year until reaching $3 million on July 1, 2031.
Removing the cap could significantly increase malpractice premiums, accelerate provider burnout, and drive specialists like OB-GYNs and pediatric providers out of already underserved regions of the state.
Simply removing the cap will also increase the amount of lawsuits and make the malpractice environment in Virginia worse.
Status: The bill was reported from the Senate’s Courts of Justice committee and re-referred to Finance and Appropriations (10‑Y 4‑N 1‑A). Further background: this bill was introduced in the 2024 and 2025 General Assembly sessions and failed to move forward in each.
Doctors as petitioners for “substantial risk orders” | HB901 (Sullivan)
The bill impacts emergency physicians by authorizing doctors and other medical professionals to petition courts for firearm “substantial risk orders” when a patient is believed to pose an imminent danger to themselves or others.
In EDs, where physicians routinely evaluate patients in mental health crisis, intoxication, or acute distress, the bill would expand their role beyond medical assessment into formal legal proceedings. Physicians’ clinical judgments and documentation could become central evidence in court — increasing administrative burdens, legal exposure, and pressure to act in high-stakes situations. Supporters argue the measure strengthens suicide and violence prevention, while critics — VACEP included — warn it risks complicating patient trust and adding new liabilities in already strained emergency care settings. Of note: Physicians would not be mandated to petition courts, but would gain eligibility to do so.
Status: The bill has been referred from the Public Safety committee and to Courts of Justice.
Authorizing physician assistants to practice independently | HB746 (Henson)
Supporters say the bill will modernize Virginia’s physician assistant practice rules by allowing experienced PAs to practice independently after completing three years of full-time clinical work under a supervising physician. Under the proposal, qualifying PAs could transition away from formal practice agreements after submitting documentation to the Board of Medicine, giving them greater professional autonomy and potentially expanding access to care, particularly in underserved communities.
However, VACEP and the Virginia Academy of Family Physicians have called for amendments to tighten oversight and limit the scope of PA independent practice. Proposed changes would:
Require all applicants to obtain formal physician attestation
Restrict independent practice to the specialty in which the PA gained experience
Eliminate alternative documentation pathways
Close potential loopholes for out-of-state license holders
“These safeguards are necessary to protect patient safety, ensure appropriate training and supervision, and prevent clinicians from moving into unfamiliar specialties without sufficient physician involvement,” said Jesse Spangler, MD, FACEP, VACEP’s president.