Three Days in D.C.: VACEP advocates in Congress
Boarding crisis, Workplace violence, and Medicare payment stability the topics of the day
Plus: issue one-pagers within, to keep you informed.
Virginia emergency medicine leaders volunteered three days in Washington this week at the American College of Emergency Physicians Leadership & Advocacy Conference. There, they and emergency physicians from every state (and D.C.) chapter, along with those from Puerto Rico and government agencies, learned about the inner workings of federal legislation and regulations and brushed up on the latest emergency medicine issues. On Tuesday, members spent the day on Capitol Hill meeting with their respective state’s federal lawmakers in the Senate and House of Representatives.
VACEP president Todd Parker, MD, FACEP was among the speakers and discussed this year's successes in Virginia, including advocating for a new law to bring 24/7 trained security to Virginia EDs to stop workplace violence, preventing NPs from gaining independent practice after only two years, and more.
Members of VACEP’s Board of Directors and other leaders from the state chapter advocated in Washington on May 2. They met with 13 lawmakers, including aides from the offices of both Virginia U.S. Senators Mark R. Warner and Timothy M. Kaine.
Easily eclipsing the accepted 10,000-steps-a-day goal, emergency physicians criss-crossed the U.S. Capitol grounds, moving from one federal office building to the next as they pushed for nationwide fixes to the boarding crisis, workplace violence, and bringing stability to Medicare's physician payment system.
Here’s the rundown on everything Virginia emergency physicians discussed, along with links to ACEP’s official issue papers.
Boarding
The issue: ED boarding has significantly increased nationwide and become a public health emergency. ACEP collected more than 140 personal stories from emergency physicians and nearly all respondents (97%) cited boarding times of more than 24 hours, with one-third stating they had patients stay more than one week, and 28% citing they had patients boarding more than two weeks. The ER safety net is on the verge of breaking beyond repair, with EDs gridlocked and overwhelmed with waiting patients.
The ask: Meeting with Congressional aides, VACEP members shared stories of patients impacted by boarding — and in some cases, dying while waiting for a transfer to a hospital that would never come.
Leaders told aides there is no one-size-fits-all solution to ED boarding due to its numerous drivers, causes, and breadth of stakeholders involved. VACEP urged legislators to sign a bipartisan “Dear Colleague” letter urging the presidential Administration to swiftly convene an ED Boarding Task Force with broad stakeholder representation.
In addition, we asked lawmakers to cosponsor Senate Bill 1346, the bipartisan “Improving Mental Health Access from the Emergency Department Act.”
The bill would address a significant component of psychiatric boarding by providing grants to EDs to increase access to follow-up psychiatric care for patients, such as expedited placement, increase tele-psychiatry support, expanded availability of inpatient psychiatric beds, increased coordination with regional service providers, and regional bed availability tracking and management programs.
WORKPLACE VIOLENCE
VACEP emergency physicians in an underwater paradise in the office of 1st District of Virginia Rep. Rob Wittman.
The issue: Two-thirds of emergency physicians report being physically assaulted within the last year.
“Some might say ’This is part of the job,’ but no, this is not and should not be part of our jobs,” VACEP treasurer Joran Sequeira, MD, FACEP told one Congressional aide. In addition to the immediate physical threat to emergency physicians and other ED personnel, workplace violence causes significant stress for healthcare providers and patients seeking treatment and contributes to job dissatisfaction and burnout.
The ask: VACEP and other ACEP chapter representatives asked legislators to establish important, common-sense procedures to protect emergency physicians, workers, and patients from violence in the healthcare workplace. In particular, we urged lawmakers to cosponsor two bipartisan bills:
The team posed for a quick photo with Virginia Sen. Tim Kaine. Kaine has long supported emergency physicians and was a sponsor of the federal Lorna Breen Act, which aims to reduce and prevent suicide, burnout, and mental and behavioral health conditions among healthcare professionals.
The “Workplace Violence Prevention for Health Care and Social Service Workers Act” (H.R. 2663/S. 1176) would take critical steps to address ED violence by requiring the Occupational Safety and Health Administration (OSHA) to issue an enforceable standard to ensure healthcare and social services workplaces implement violence prevention, tracking, and response systems.
The “SAVE Act” (H.R. 2584) establishes federal penalties for violence against healthcare workers, criminalizing intentional assault or intimidation against them while ensuring reasonable protections for individuals who may be mentally incapacitated due to illness or substance use. It also provides grants to healthcare facilities to implement and improve workplace violence-prevention efforts.
MEDICARE PHYSICIAN PAYMENT STABILITY
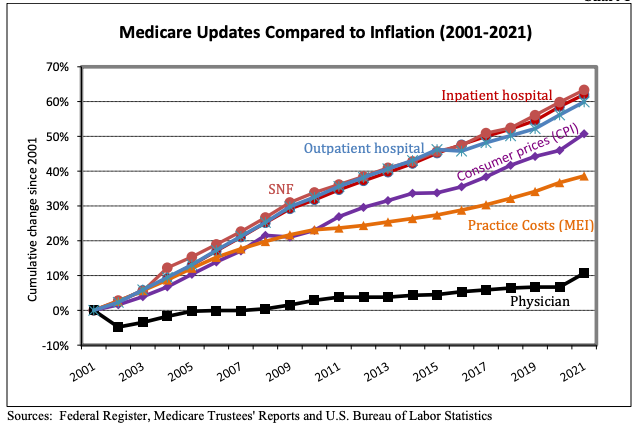
Medicare payments decreased by 53 percent when compared to inflation between 1992 and 2016. As seen in the chart, over the course of the last 20 years, the payment systems for other Medicare provider types like hospitals and skilled nursing facilities (SNFs), as well as actual practice costs reflected in the Medicare Economic Index (MEI), have far exceeded Medicare payments under the Physician Fee Schedule.
VACEP’s Jesse Spangler, MD, FACEP (left) and Todd Parker, MD, FACEP (right) with Emergency Medicine Residents Association president Jessica Adkins Murphy, MD and ACEP President Christopher Kang, MD, FACEP. Kang spoke to VACEP members at the annual CME Conference in February. See his remarks here.
The issue: For decades, Medicare physician reimbursements have failed to keep up with inflation, despite other Medicare participants receiving annual inflationary updates. Further, the yearly threat – and implementation – of significant cuts to Medicare physician payments continues to destabilize the healthcare safety net. EDs across the country have not fully recovered from the pandemic and struggle under the weight of the boarding crisis. Rather than face a yearly scramble to address steep payment cuts, emergency physicians want long-term stability for Medicare beneficiaries and the physicians who manage and provide their care.
The ask: Essentially, tie increases to pay to inflation. The “Strengthening Medicare for Patients and Providers Act” (H.R. 2474) would bring much-needed stability and establish an inflationary update in the Medicare Physician Fee Schedule (PFS) based on the Medicare Economic Index (MEI). More details in the one-pager (at the button).
A special thanks to the offices of Virginia’s representatives for meeting with Virginia emergency physicians this week and giving us ample time to explain our issues.
VA-01 Rep. Rob Wittman (R)
VA-02 Rep. Jennifer Kiggans (R)
VA-03 Rep. Bobby Scott (D)
VA-O4 Rep. Jennifer McClellan (D)
VA-05 Rep. Robert Good (R)
VA-06 Rep. Ben Cline (R)
VA-07 Rep. Abigail Spanberger (D)
VA-08 Rep. Donald Beyer (D)
VA-09 Rep. Morgan Griffith (R)
VA-10 Rep. Jennifer Wexton (D)
VA-11 Rep. Gerry Connolly (D)
VA-S Sen. Mark Warner (D)
VA-S Sen. Tim Kaine (D)