Optimistic ACEP President Schmitz addresses Virginia emergency docs, covers four “challenges and opportunities” in EM
Stay optimistic. We’ve been here before, and we’ll get through it again.
ACEP President Gillian Schmitz, MD, FACEP addresses a room of Virginia emergency physicians at The Omni Homestead Resort on Feb. 12, 2022.
That was the message delivered to a room of Virginia emergency physicians by ACEP President Gillian Schmitz, MD, FACEP. In considering the four big “challenges and opportunities ahead” for emergency medicine, Schmitz echoed the spirit of her favorite TV hero, Ted Lasso, and his positivity and drive to win in the face of mounting pressures.
“I’m asking you to come at this with a sense of optimism that we’re going to be okay,” Schmitz told members of the Virginia College of Emergency Physicians at The Omni Homestead Resort in Hot Springs, Va. for the group’s Annual CME Conference. “I know people are stressed right now, I know there's a high level of anxiety about multiple different factors impacting our practice, but it's going to be okay, and we’re making some significant headway.”
Here are the four EM issues she covered.
Workforce
With the supply of EPs expected to outpace demand for the specialty within 10 years, Schmitz said it’s important to stop the proliferation of EM residency programs and reduce the acceptance rate to them — both of which have grown significantly in the past decade.
In 2011, about half of applicants were placed in an EM residency. In 2020, 71% of students were accepted. One approach is to de-emphasize EM residencies and push med students to focus on specialties with residency and doctor shortages, she said.
It’s already starting. There’s been about a 10% decrease in EM residency applications nationwide, she said. “We want it to go down, but we don’t want it to go down too much,” she says. “We want to be one of the more competitive specialties.”
Scope of Practice
When it comes to independent practice of advanced-practice providers, especially in EDs, ACEP takes a hard line.
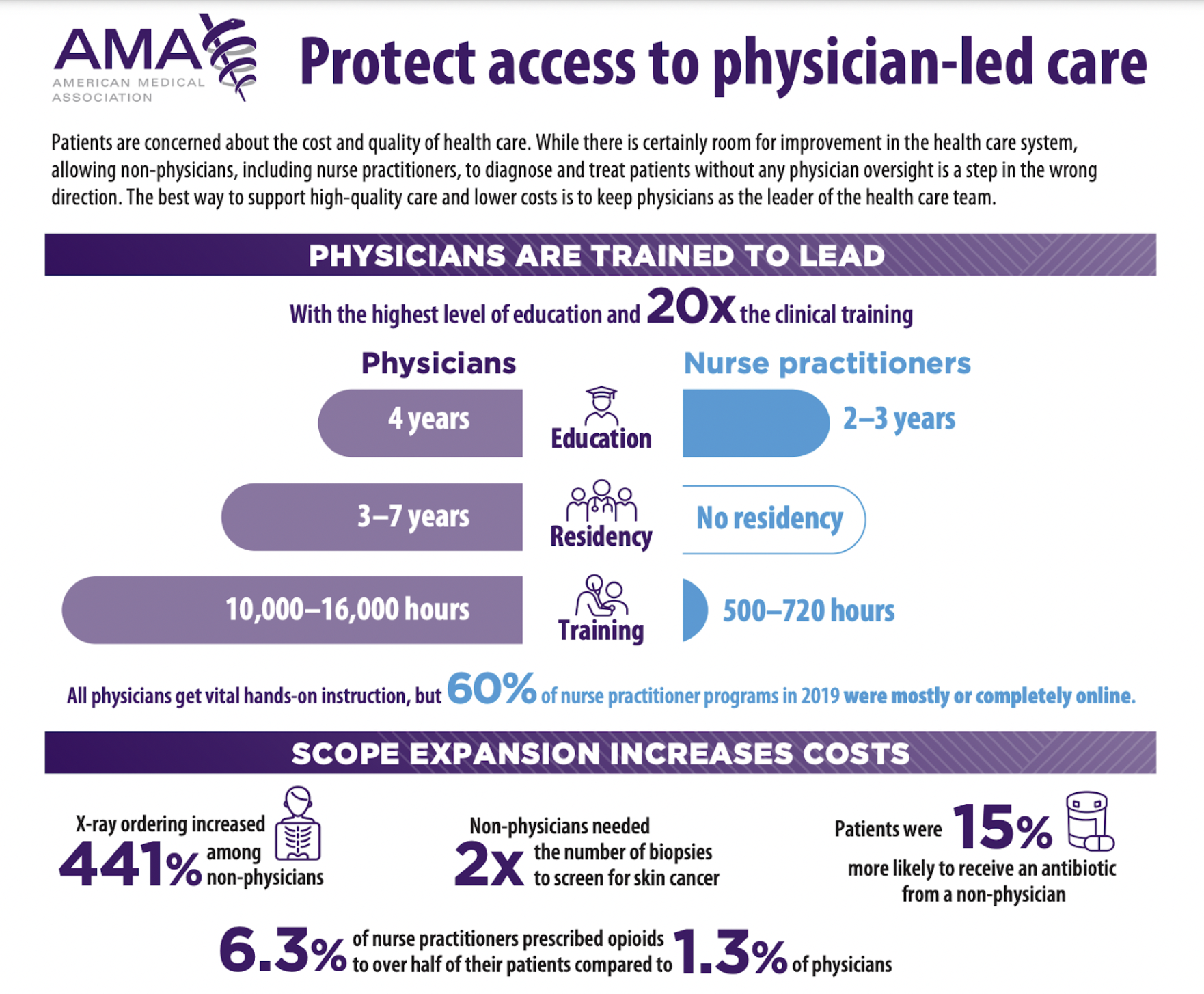
Schmitz shared this infographic from the American Medical Association while discussing scope of practice issues.
“We support team-based care. There is a role for everyone who plays in the ED, but we absolutely and vehemently support physician-led care. Every patient deserves to have physician input into their care,” Schmitz said. “This is an absolute core [belief], that our training and education matters. You don’t know what you don’t know. And this is why the value of our training and education is really important to dictating care.”
The fact remains, however, that about 25% of all ED patients see a PA or NP, she said. Medicare data shows an increasing number of patients are being seen by advanced-practice providers even in higher acuity cases, she said.
ACEP is fighting scope of practice bills in numerous states. Some have been successful. Others have put strong restrictions on practice guidelines, like in Virginia, where NPs require five years of training before being able to practice independently (though a bill in Virginia would change this to only two years). Schmitz said ACEP is also focusing on carveouts for emergency departments that would prevent PAs and NPs from practicing independently in “environments that are not really appropriate for somebody with less training to be taking care of patients,” she said.
ACEP is also reviewing the definition of adequate supervision for advanced-practice providers, she said.
Changing landscape of medicine
As much as physicians don’t like to talk about it, healthcare is a business and a leading economic sector, Schmitz says.
“Wherever there is profit to be had, private equity is going to get involved,” she said. In addition, the industry has witnessed rapid consolidation of insurance companies, hospitals, and health systems in their efforts to build market share. Capturing such economies of scale helps reduce costs, meet regulatory demands, and pay competitive salaries.
The changes, Schmitz explained, are driven by continual threats to reimbursements in a marketplace of razor-thin margins.
Whether through consolidation or practice ownership by contract management groups, physicians — emergency or otherwise — fear they are losing autonomy and the ability to make decisions at a local level, Schmitz said. Yet when it comes to private equity and joining a large contract-management group, she admitted there can be benefits, particularly when it comes to negotiating with insurance companies.
“I'm not saying that I like it. But I'm saying this is the reality we are in,” she said. “And we need to start adapting and preparing for that future. It's going to make it increasingly difficult for small groups to be able to compete in our current reimbursement market.”
She compared emergency medicine’s current position to that of Blockbuster Video stores prior to Netflix and streaming services. “We don’t want to end up like Blockbuster,” she said, landing a joke that all the old video-rental stores are now freestanding EDs. “We have to understand the reality of the landscape around us, and the different stakeholders and things that are changing the market.”
And emergency physicians must also recognize they are but one component in the foundation of a hospital, where the majority of them practice.
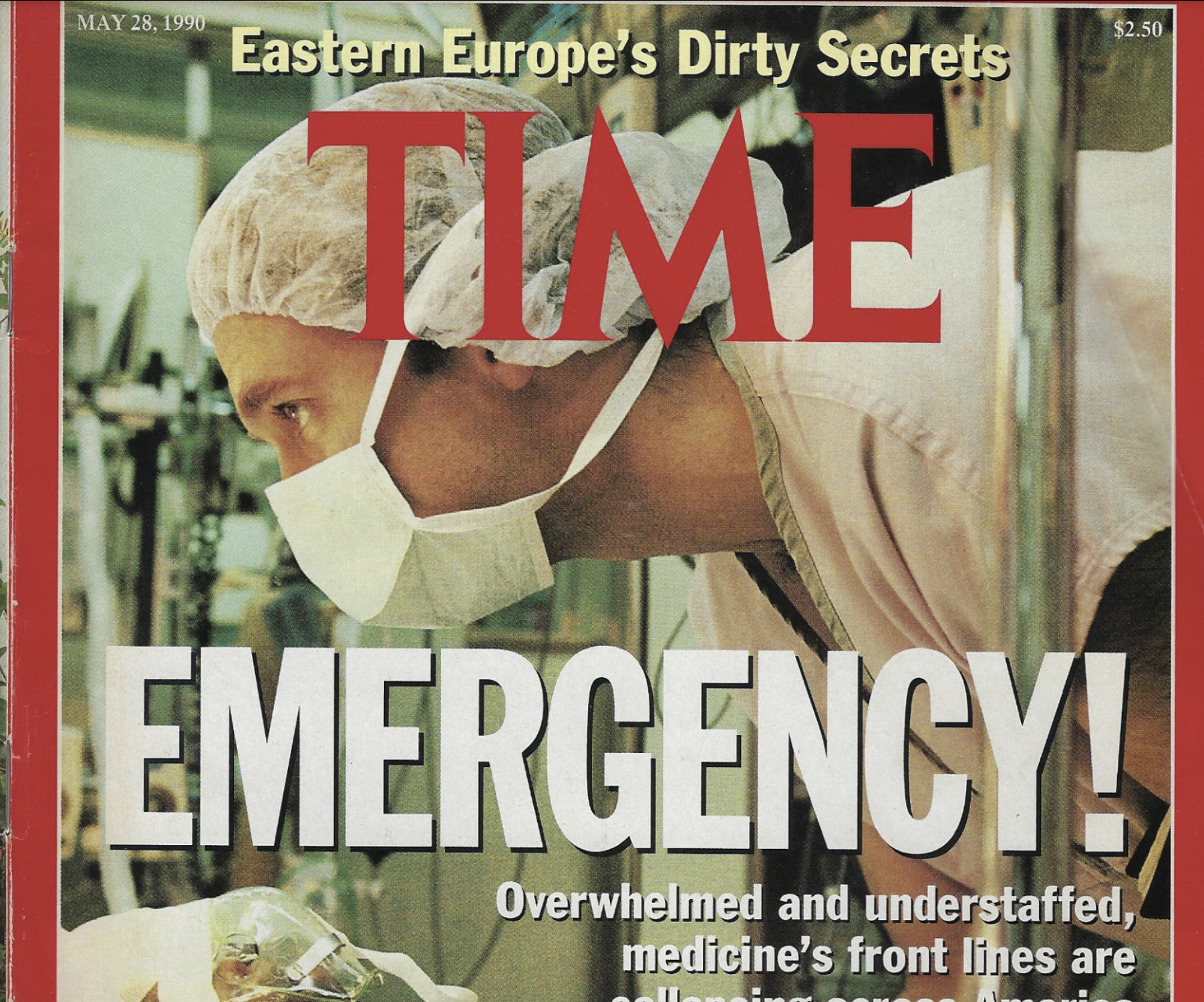
Schmitz shared this 1990 Time magazine cover story, which covered burnout and overwhelmed EDs. “The more things change, the more things stay the same,” she said. “We've beaten these odds before. This has come up multiple times where people thought the sky was falling emergency medicine was over,” she said. “And we've gotten through it every single time, because we're resilient, because the country needs us, because we provide a central service to anyone, anywhere, anytime.”
“You can have a fantastic ED group, with no complaints. They're at the top of their quality scores, great medical staff. But it's hard for them to compete when another contract group comes in and says [to hospital administrators], ‘We can do that. We can also do your hospitalists, we can also do your intensivists.’ And hospitals are more and more going to those larger groups and contracts because it saves so much. It brings in higher reimbursement for them, it gives them potentially less costs.”
But at what cost? “That's what we're trying so hard to answer,” Schmitz says. She noted ACEP has not been able to find any objective data that looks at the impact of consolidation on costs and care quality in the ED.
She also acknowledged that consolidation and private equity investment trends are bigger than ACEP.
“There is no easy button to address the market forces — you have to fundamentally address the reimbursements that cause those market forces and that consolidation,” she said. “The way we fund healthcare has to change, because what we’re doing is not sustainable. But until we address the bigger market forces and the bigger reimbursement issues, I think further consolidation is likely inevitable.
She said ACEP is working at the federal level to push for legislation that upholds due process for physicians, giving practitioners the ability to advocate by avoiding the mandatory waiver of due process rights which many are forced to comply with as a condition of group employment. ACEP is working with CMS to enforce more transparency in Medicare billing. They are also considering an ACEP accreditation for EDs, looking at best practices, standards of care, and staffing ratios.
“Taking on a challenge is a lot like riding a horse, isn’t it? If you’re comfortable while you’re doing it, you’re probably doing it wrong. ”
Reimbursement
Finally, Schmitz hit on reimbursement issues, specifically around the years-long legislative process to end balance billing and the negative news stories that, however misleading, blame emergency physicians for large patient medical bills.
ACEP led the charge to pass the federal No Surprises Act in December 2020. The law is designed to protect patients from surprise out-of-network bills.
The law created a fair independent dispute resolution (IDR) process in cases where physicians and insurers could not agree on a fair rate. The process requires an arbiter to consider all information submitted by the two parties, including the median in-network rate, complexity of the case, previously contracted rates and market power of the physician and insurance company, among other things.
Although the law intended to resolve payment disputes through this impartial arbitration system, an “interim final rule” released in 2021 by the Departments of Health and Human Services, Labor, and Treasury created a system that empowers profit-seeking insurance companies to strong-arm local community physician practices, narrow their provider networks and reduce access to care.
ACEP has filed a lawsuit against the federal government, arguing that the interim rule goes against the language of the No Surprises Act and will ultimately harm patients and access to care.
Despite the challenges – and opportunities – in emergency medicine, Schmitz wrapped her keynote by showing the cover of a 1990 Time magazine with a headline about overwhelmed and overstaffed EDs that warned of a collapsing system.
But emergency physicians got through it 30 years ago, and we’ll get through it today, she said. And she reminded everyone:
“What you do has purpose. What you do is important, is insightful, and is critically important to the well-being of not only our patients but to the hospital and healthcare system of our country. You're not only saving lives, but you're changing policy, you're changing advocacy, you're changing the ways we deliver and protect care for an entire country.”