VACEP's EBM Review Series: Reducing Unnecessary Blood Cultures Using a Clinical Decision Rule
VACEP Evidence-Based Medicine for General Emergency Physicians Series
Authors: Ryan Danko, MD PGY-3 & Jordan Tozer, MD | VCU Health
Reviewer: Christopher Fahlsing, MD, PGY4 & Dean Cataldo, DO (LT, MC, USN) | Naval Medical Center Portsmouth
The VACEP Evidence-Based Medicine Review Series allows Virginia emergency medicine residents and attendings to share and analyze a recent peer-reviewed clinical study. You can also read the full article, “A clinical decision to rule out bloodstream infection in the emergency department: retrospective multicentric observational cohort study,” from the Journal of Emergency Medicine December 2024 edition.
THE CASE
A 32-year-old man with no past medical history presents for evaluation of myalgias, cough, and a sore throat for 2 days. Triage vitals are significant for tachycardia to 125 bpm and a fever of 101.2F. He has a normal blood pressure.
Your staff notifies you that your patient meets criteria for a sepsis alert; should you obtain blood cultures?
IMPACT OF BLOOD CULTURES
Figure 1. Shapiro, et al. criteria to evaluate for bacteremia utilizing lab work.
Blood cultures are an essential tool for evaluating bacteremia in the overall evaluation of sepsis, especially for high-risk patient populations. However, inappropriately obtained cultures can be contaminated, and obtaining cultures is associated with an increased length of stay.
Blood cultures are ordered on 7.8% of ED admissions. 2
5.1% of blood cultures are falsely positive (contaminants). 2
14.4% of patients with blood culture collection have clinically relevant bacteremia. 2
Blood cultures require additional straight sticks.
Blood cultures are in shortage nationwide.
Clinical decision tools have been created with high sensitivity for bacteremia. In 2008, Shapiro et al. proposed a clinical decision tool that evaluated the need for blood cultures with 97% sensitivity and 99.1% negative predictive value. If implemented in their data set, blood cultures would be reduced by 27%.
Unfortunately, Shapiro et al. and other clinical decision rules require laboratory blood testing and are not widely used in practice. 3 Sometimes, it is not practical to follow up on lab results and then decide to obtain cultures after the fact.
STUDY SUMMARY
Pehlivan et al. sought to evaluate risk factors for bacteremia without blood draws for laboratory testing. A retrospective cohort was chosen from 2017 to 2019, resulting in 2580 included patients. All patients with blood cultures obtained and admitted to Angers University Hospital in France or Cliniques Universitaires Saint-Luc in Belgium were evaluated for bacteremia. 75% of these patients were randomly assigned to the derivation cohort and 25% to a validation cohort. Patients who had positive cultures with common skin contaminants (coagulase-negative staph, strep viridans, etc.) and were not treated with a course of antibiotics were considered contaminants; these were considered negative cultures for the study.
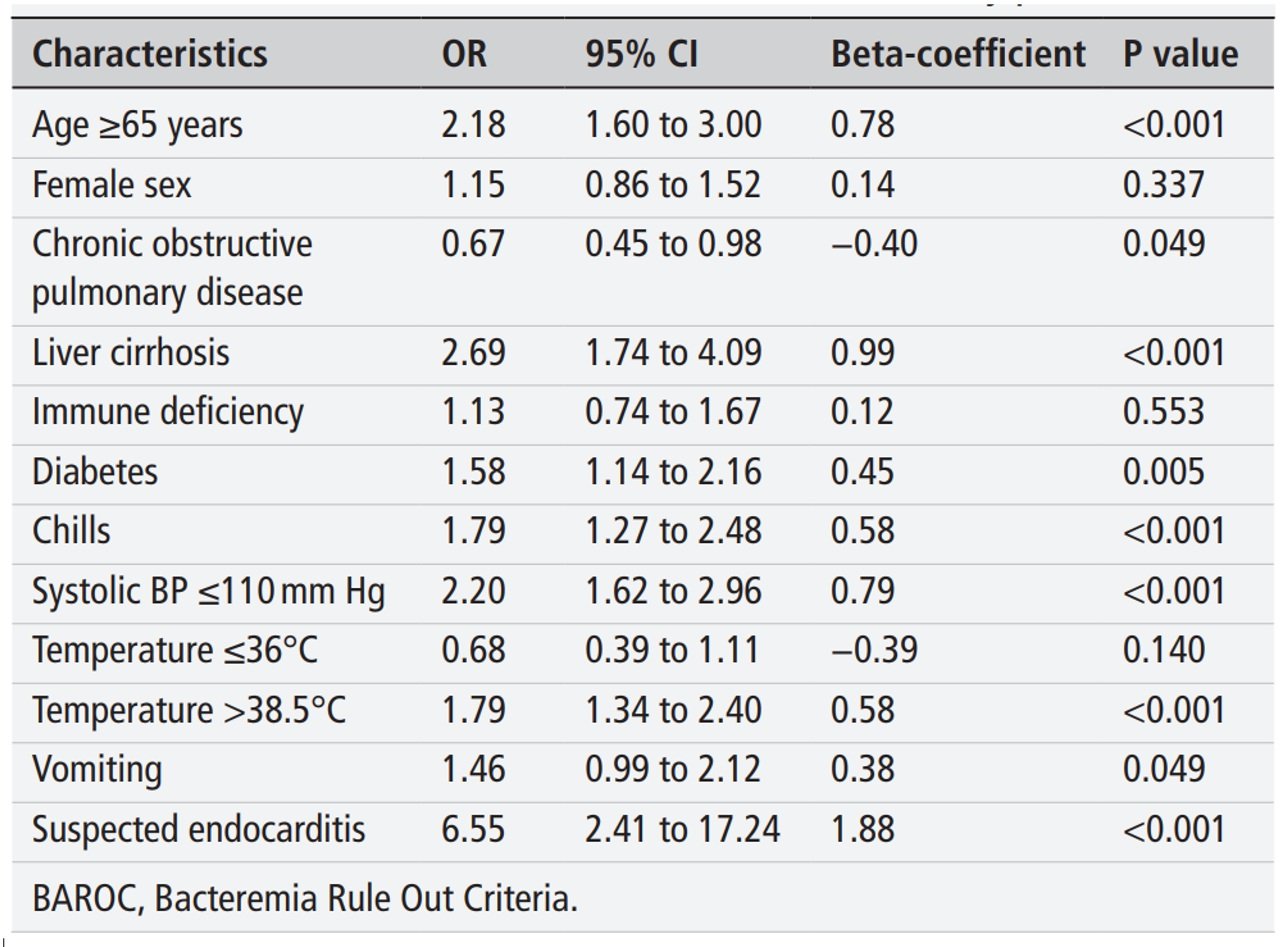
Figure 2. BAROC Criteria for the formula
Clinical risk factors associated with bacteremia were identified in the derivation cohort and assigned odds ratios, creating what the authors termed the “Bacteremia Rule Out Criteria” (BAROC) score. The primary endpoint was the rate of bloodstream infections in the validation arm patients with a negative BAROC score. Based on historical risk factors, vital signs, and symptoms, this scoring tool was 97% sensitive (95% CI 95% to 100%) with a negative predictive value of 100% (95% CI 94% to 100%). A second arm of the validation cohort included laboratory data, increasing sensitivity to 100% (95% CI 94% to 100%) while NPV remained unchanged. The authors conclude that the BAROC score can safely identify patients at low risk for bacteremia without labwork, therefore reducing unnecessary blood culture collection. However, it should be noted that when lab values were added to the validation cohort (n=570), while the model’s accuracy increased - it was not statistically significant (p=0.6). Which argues that the non-lab BAROC is an even more efficient use of the model as a screening tool - especially when the patient doesn’t require labs for risk stratification.
About the EBM Review Series
This is a literature review series started by the University of Virginia’s Josh Easter, MD, MSc, a VACEP board member working to connect the academic community in Virginia. We invite each residency in Virginia (and D.C.) to create a faculty/resident team to submit and review articles. Sign up to submit one.
Goals
Provide a brief monthly synopsis of a high yield article germane to the practice of emergency medicine for distribution to all VACEP members
Provide an opportunity for a peer reviewed publication and invited presentation for faculty and trainees
Foster an academic community focused on evidenced based medicine for emergency medicine residency programs in the region
LIMITATIONS
This study has several limitations:
The classifications of contaminants may have led to an underestimation of true bacteremia and falsely elevated sensitivity.
Only patients who were admitted in the first week of the month were included which may underrepresent seasonal variability leading to convenience sampling.
Patients were only included in the study if the clinician ordered blood cultures leading to sampling bias.
Not all patients included in the study had two sets of blood cultures obtained; this could again reduce the incidence of bacteremia in the study.
This study has not undergone external or prospective validation.
CASE CONCLUSION
Based on our patient’s clinical history, we utilized the BAROC clinical decision tool (https://ceral-chu-angers-49.shinyapps.io/BAROC/), which calculated a 1% risk of having a bloodstream infection and therefore recognized that we do not need to obtain blood cultures.
DISCUSSION
Emergency physicians are accustomed to balancing risks with benefits and being cost-conscious with regard to diagnostic testing. This is even more pronounced in resource-limited settings or situations where resource utilization is scrutinized, such as in the current blood culture shortage.
The authors of this study created a scoring tool using risk factors and symptoms that may seem intuitive, which is a potentially useful clinical tool that can help reduce the number of blood cultures drawn. Consequently, this may reduce unnecessary blood draws, false positive contaminants, hospital admissions, and unnecessary antibiotic use.
There are multiple screening tools focused on high sensitivity to prevent missing sepsis (SIRS/qSOFA/NEWS2); these additionally lead to increased fluids, antibiotics, and blood cultures to meet CMS sepsis bundles for reimbursement. The BAROC score can work as another layer in synergy to add specificity to our sepsis alerts. For every patient who meets sepsis criteria, we do not blindly give 30cc/kg of fluids. The BAROC score justifies with evidence-based medicine why healthy patients do not need blood cultures and could be used to help meet surviving sepsis campaign protocols (SEP-1).
REFERENCES:
1. Pehlivan J, Douillet D, Jérémie R, et al. (2024) A clinical decision rule to rule out bloodstream infection in the emergency department: retrospective multicentric observational cohort study. Emergency Medicine Journal 41, 20-26. https://doi.org/10.1136/emermed-2022-212987 | https://pubmed.ncbi.nlm.nih.gov/37940371/
2. Rothe K, Spinner CD, Ott A, Querbach C, Dommasch M, Aldrich C, et al. (2019) Strategies for increasing diagnostic yield of community-onset bacteraemia within the emergency department: A retrospective study. PLoS ONE, 14(9). e0222545. https://doi.org/10.1371/journal.pone.0222545 | https://pubmed.ncbi.nlm.nih.gov/31513683/
3. Eliakim-Raz, N. et al. (2015) Predicting bacteraemia in validated models—a systemic review. Clinical Microbiology and Infection, 21(4), 295-301. www.clinicalmicrobiologyandinfection.com/article/S1198-743X(15)00249-9/fulltext | https://pubmed.ncbi.nlm.nih.gov/25677625/
4. Shapiro, Nathan L. et al. (2008) Who Needs a Blood Cultures? A Prospectively Derived and Validated Prediction Rule. Journal of Emergency Medicine, 35(3), 255-264. www.jem-journal.com/article/S0736-4679(08)00444-7/ | https://pubmed.ncbi.nlm.nih.gov/18486413/
Disclaimer: The views expressed in this review article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. We are military service members. This work was prepared as part of our official duties. Title 17 U.S.C. 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person’s official duties.